Abstract
Introduction : Portal vein thrombosis (PVT) is an unusual-site thrombosis mainly encountered in patients with malignancies, cirrhosis, myeloproliferative disorders (MPN) and acute abdominal inflammatory conditions (AIC). Given the associated comorbidities that can increase bleeding risks in this heterogeneous population, management is challenging. Current recommendations suggest that anticoagulation improves recanalization rates but there is limited information on venous thromboembolism (VTE) recurrence rates and whether the varied etiologies of PVT fare similarly with anticoagulation.
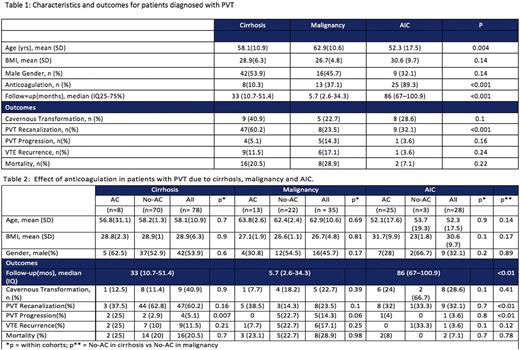
Aim: To compare the anticoagulation rates of patients with PVT in patients with cirrhosis, malignancy and AIC and to determine its effect on clinical outcomes of cavernous transformation, recanalization, PVT progression, PVT recanalization, VTE recurrence and mortality.
Methods: Approval was obtained from Montefiore Institutional Review Board to review records of patients from 2005 to 2015. Institutional data mining software was used to identify patients diagnosed with PVT and their etiologies by ICD9 and the index exam results were reviewed manually to ensure accuracy. Results regarding cavernous transformation, PVT recanalization and progression were acquired directly from follow-up imaging studies; data regarding VTE recurrence, mortality and anticoagulation were obtained from chart review. For the purposes of this study, patients with imaging confirmation, imaging follow-up and a diagnosis of cirrhosis, malignancy or AIC were selected. AIC was defined as abdominal infections, acute intra-abdominal surgical procedures or bacteremia occurring within 60 days preceding PVT diagnosis.
Results: 698 patients were diagnosed with PVT. Among them, 198 (28.4%) had cirrhosis, 151 (21.6%) had malignancy and 35 (5%) had AIC. Of these, 141 patients had follow-up and were included in the analysis; 78 patients with cirrhosis, 35 with malignancy and 28 with AIC. The mean age was 58.1 ± 12.8 years, 38.8% were Hispanic and 29.6% were African-American and the AIC cohort was the youngest at 52.3yrs. The median follow-up was 35 months.
Only 32.6% of patients received anticoagulation. Patients with malignancy were anticoagulated more frequently compared to those with cirrhosis (37.1% vs 10.3%, p<0.001) but patients with AIC were placed on anticoagulation most often (89.3%, p<0.001). Cirrhotic patients that were anticoagulated had higher PVT progression rates than those not anticoagulated (25% vs 2.9%, p<0.05) and we did not detect a significant benefit of anticoagulation in PVT recanalization, decreased recurrence or lower mortality rates for patients within cohorts of either the cirrhosis or the malignancy groups. AIC patients did have a lower rate of VTE recurrence with AC (0/25 as compared to 1/3) but the numbers were small. Comparing patients that did not receive anticoagulation across cohorts, recanalization rates were higher and progression rates were lower for patients with cirrhosis versus malignancy (62.8% vs 14.3%, p<0.001 for recanalization; 2.9% vs 22.7% for progression, p=0.002). PVT recanalization rate was also higher when compared to patients with AIC, no matter the therapy (32.1% vs 60.2%, p<0.001).However, there was a trend towards increased rates of cavernous transformation in PVT patients with cirrhosis compared to patients with AIC or cancer (40.9% for cirrhosis vs 22.7% for malignancy and 28.6% for AIC, p=0.1).
Conclusion: Despite lower rates of anticoagulation, patients with cirrhosis were more likely to achieve recanalization and did not have an increased risk of recurrence, progression or mortality compared to other groups. Patients with AIC were younger than those with cirrhosis and malignancy and were more likely to get anticoagulation; however, this did not correlate with higher PVT recanalization or lower progression, recurrence or mortality rates. PVT is associated with multiple pathologies; one therapy for all causes of PVT may not be beneficial.
Billett: Janssen Pharmaceutical: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.